Infertility
Risk Factors for Pid and Infertility
We have the complete source for total info and resources for Risk Factors for Pid and Infertility online.
Atrophy is observed within 1-6 months, and the degree of atrophy does not correlate with the severity of orchitis or infertility. For this reason, it’s recommended that couples who’ve been trying to get pregnant for over a year without success seek the advice of a doctor.
Cushing disease Increased cortisol levels cause a negative feedback on the hypothalamus, decreasing GnRH release. Source : Infertility and its Treatments - PPT Presentation Summary : Infertility and Its Treatments.
Here are Some More Information on Lecture on Infertility
More Resources For Risk Factors for Pid and Infertility
1) Advancing maternal age: Historically before the latter 20th century, women were conceiving in their teens and twenties, when age-related abnormalities with the egg were not evident. Existing definitions of infertility lack uniformity, rendering comparisons in prevalence between countries or over time problematic. Primary vs. secondary infertility[edit] Primary infertility is defined as the absence of a live birth for women who desire a child and have been in a union for at least 12 months, during which they have not used any contraceptives.[14] The World Health Organisation also adds that 'women whose pregnancy spontaneously miscarries, or whose pregnancy results in a still born child, without ever having had a live birth would present with primarily infertility'.[15] Secondary infertility is defined as the absence of a live birth for women who desire a child and have been in a union for at least 12 months since their last live birth, during which they did not use any contraceptives.[15] Thus the distinguishing feature is whether or not the couple have ever had a pregnancy which led to a live birth. Isolated FSH deficiency This is a very rare cause of infertility.
More Resources For Lecture on Infertility
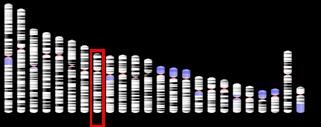
Human male infertility, the Y chromosome, and dinosaur extinction. (PDF, 1 MB) Middle East Fertility Society Journal, January 18, 2011.Oath und seine Partner benötigen Ihre Einwilligung, um auf Ihr Gerät zuzugreifen und Ihre Daten (einschließlich Standort) zu nutzen, um mehr über Ihre Interessen zu erfahren, personalisierte Anzeigen bereitzustellen und deren Effektivität zu messen. Transvaginal ultrasound – Ultrasound is an important tool in evaluating the structure of the uterus, tubes, and ovaries. Semen is the milky fluid that a man's penis releases during orgasm. Hormonal Problems A small percentage of male infertility is caused by hormonal problems. The hypothalamus-pituitary endocrine system regulates the chain of hormonal events that enables testes to produce and effectively disseminate sperm. Several things can go wrong with the hypothalamus-pituitary endocrine system: · The brain can fail to release gonadotrophic-releasing hormone (GnRH) properly. GnRH stimulates the hormonal pathway that causes testosterone synthesis and sperm production. A disruption in GnRH release leads to a lack of testosterone and a cessation in sperm production. · The pituitary can fail to produce enough lutenizing hormone (LH) and follicle stimulating hormone (FSH) to stimulate the testes and testosterone/sperm production. LH and FSH are intermediates in the hormonal pathway responsible for testosterone and sperm production. · The testes� Leydig cells may not produce testosterone in response to LH stimulation. · A male may produce other hormones and chemical compounds which interfere with the sex-hormone balance.
Below are Some More Information on Homeopathy Causes Infertility
After a woman ovulates, her body temperature rises by as much as 0. The Prevention of Acute Tubular Necrosis in Renal Transplantation by Chronic Salt Loading of the Recipient. (PDF, 627 KB) ANZ Journal of Surgery, 1974. Blood test: The lab will test for levels of testosterone and other hormones. The NICE guidance has more about unexplained infertility. There are also a number of sperm production problems that can contribute to infertility, including: Scrotal varicose veins (varicoceles) Scrotal varicose veins (varicoceles) are swollen veins causing your testicles to get hotter and affect the production of sperm These are treated with surgery Testicular injury Serious trauma to the testicles such as becoming twisted (torsion) can affect sperm production Damage from playing sports or an accident can rupture the vessels that supply blood to the testicles Previous injuries can’t be treated, but an ART treatment may help you to conceive Undescended testicles In the uterus, baby boys’ testicles form in their abdomen and descend into their scrotum shortly before birth Some men’s testicles don’t descend before they are born (cryptorchidism), although in these cases they usually drop in the first six months after birth If left untreated, undescended testicles can affect fertility Testicular cancer This happens when a malignant tumour in the testicle destroys testicular tissue If undetected, testicular cancer can spread to other parts of the body This is treated either by surgery, medication, radiotherapy or chemotherapy However, cancer therapy can also damage sperm production Genetic defects Sometimes, genetic information on the Y chromosome (which is only present in men) is deleted (micro-deletions),6 which can reduce the production of sperm Depending on where the micro-deletion is on the chromosome, this may be treated by surgically extracting sperm from part of your reproductive tract However, some couples may need to consider using a donor sperm to conceive Mumps Contracting mumps (or mumps-related orchitis) after puberty may damage the sperm-producing cells in your testicles, causing infertility or subfertility7 Usually, only one testicle is affected and if you have one functioning testicle you may not need treatment However, some couples may need to use a sperm donor in order to conceive Anti-sperm antibodies Anti-sperm antibodies are large proteins in your blood that are hostile to sperm They can cause sperm to clump together and prevent them from swimming, or they may mistake sperm cells for an infection and try to destroy them This can be treated using an ART treatment Lifestyle Sperm production can be affected by a range of lifestyle factors, including smoking, drinking, drugs, stress, overweight and unhealthy food Environmental factors can also affect your sperm quality, including overheating of your testicles, some sexual lubricants, the chemicals involved in certain manufacturing, painting or printing jobs These factors are treated by making lifestyle changes, such as wearing loose clothing to avoid overheating Hormonal problems Hormonal problems are rarely the cause of male infertility problems However, some men have a natural deficiency in follicle-stimulating hormone (FSH) and luteinising hormone (LH), which prevents the testicles from producing testosterone or developing healthy sperm Hormonal problems can usually be treated with medication Obstruction problems Blocked sperm ducts Occasionally, male sperm ducts (epididymis and vas deferens) can become blocked, meaning that your semen doesn’t contain any sperm This can be treated with surgery, or sperm may be surgically extracted from part of your reproductive tract Vasectomy Some men have had a previous vasectomy to stop them being able to conceive This can sometimes be reversed using surgery The procedure’s success depends on how long ago your vasectomy was performed Previous infections Infections can cause scarring or adhesions (organs sticking together) in your sperm ducts This can usually be treated with surgery Does age affect male fertility? Assessment of efficacy of varicocele repair for male subfertility: a systematic review. 50% are female causes with 25% being due to anovulation and 25% tubal problems/other.[74] In Sweden, approximately 10% of couples wanting children are infertile.[75] In approximately one third of these cases the man is the factor, in one third the woman is the factor, and in the remaining third the infertility is a product of factors on both parts. Sperm can survive inside the female for up to 5 days, while an egg can be fertilized for up to 1 day after ovulation. A small Steering Committee with six Expert Working Group Chairs, local Swiss experts, as well as Presidents, Chairpersons and representatives of ASRM1, ESHRE2, FIGO3, GFMER4, ICMART5 and IFFS6 came to the table to share experiences, to present their current (or in-process) guidelines and to recommend a collaborative process for moving forward to generate global guidelines. A smaller amount may suggest a structural or hormonal problem leading to deficient semen production; 2) sperm concentration – normal concentration should be at least 20 million sperm per 1 ml of semen. 17 Evaluation of male infertility starts with a history and physical examination focusing on previous fertility, pelvic or inguinal surgeries, systemic diseases, and exposures. The initial dosage of clomiphene is 50 mg daily for five days starting on day 3 to 5 of the menstrual cycle.
Previous Next
See also
Infertility Supervision Icd 10
Management of Infertility in Ghana
Anovulatory Infertility and Fertility